Pharmacy Optimization Tools
13 tools to use when planning for pharma scale-up
1. Plan for FDA approvals
Only 12% of drugs that make it from the lab and into phase 1 clinical trials end up receiving FDA approval. However, planning for eventual pharma scale‑up long before you receive approvals allows you to achieve commercial‑scale production in the quickest possible timeframe.
Assess your facilities and capabilities in preparation: ensure you have the equipment capacity and floor space to meet production volumes, have enough consumables on‑hand for the first batches, train your workforce, and prepare your supply chain.
This strategy is not as risky as it may seem. Investing in these areas early on means that you will be ready for commercial production as soon as possible once you receive your approvals, avoiding long periods of downtime as you design new facilities and validate processes. The increased uptime quickly compensates for the initial investments.
Remaining risks can be mitigated by using flexible, small‑volume manufacturing techniques which scale easily and sufficiently to meet the production demands of even phase 3 clinical trials. Additional scale‑up processes can be designed in parallel with those late‑phase trials.
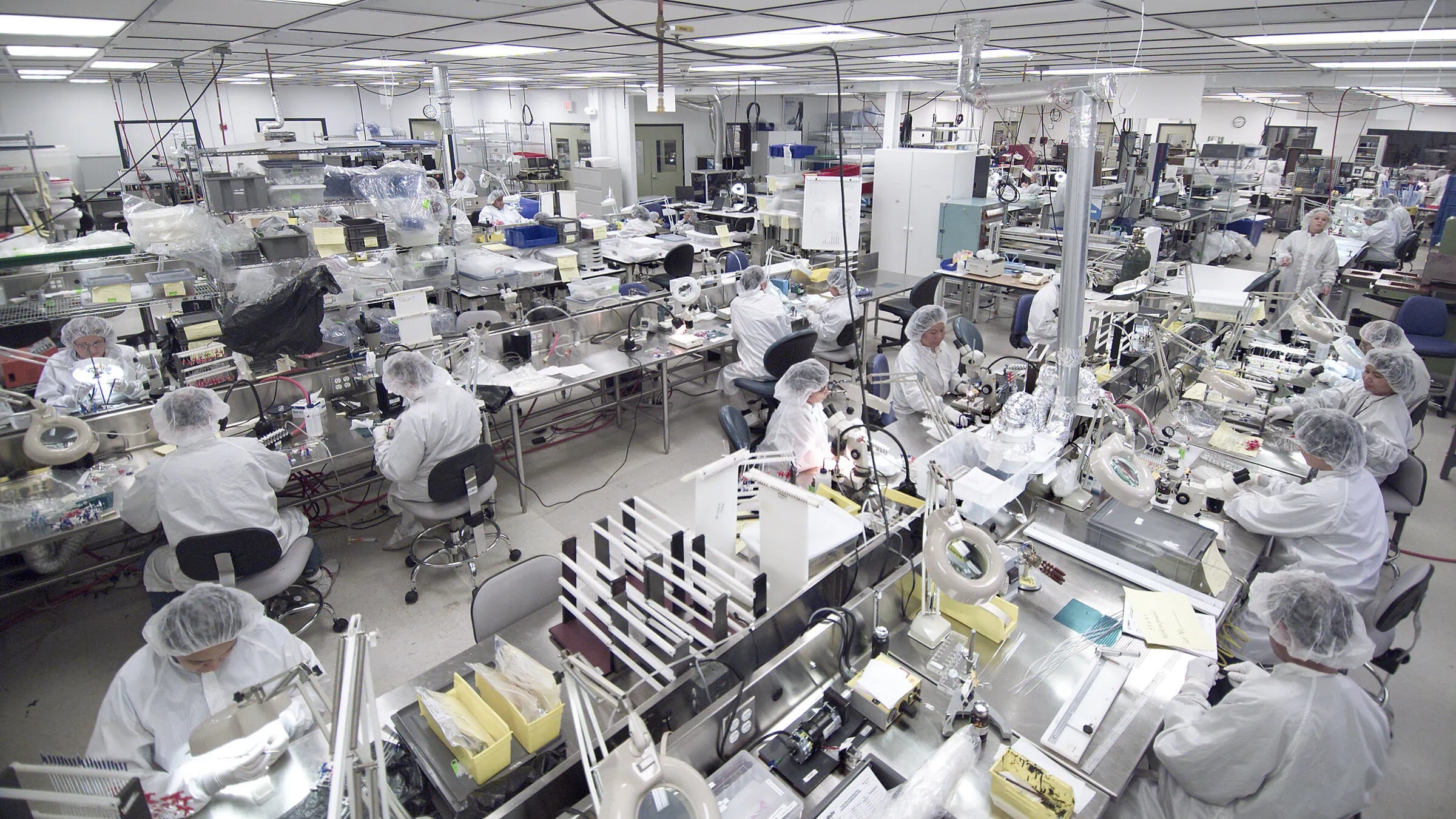
2. Design for commercial production in a GMP cleanroom
Design choices made early in the development process can significantly affect your speed to market, regulatory compliance, and flexibility for future growth. Considering factors that will be necessary for high‑volume manufacturing while you are still working in an R&D lab can save you from months of work down the line.
Then, as your process develops, you can choose a specialized CDMO to design a new process, new equipment, and/or a new facility, all of which can be designed for maximal uptime at every process phase. This can be as simple as ensuring easy‑access to pieces of equipment that require regular service, so technicians can quickly and easily make the needed repairs — minimizing downtime. Any higher costs (for instance, those for preventative maintenance) will be offset by the increased uptime.
3. Strengthen your supply chain
Standard means of de‑risking a supply chain are powerful tools to make sure that your vendors don’t become a bottleneck to successful scaling. Check that your suppliers will be able to support the higher volumes necessary for production, and find a second source when necessary. While qualifying a new supplier is time consuming and expensive, doing it early will prevent later supply chain and regulatory delays, when you would much rather be focusing on scale-up.
4. Classic lean manufacturing: it’s not just for Toyota
Lean has been rigorously applied to pharmaceutical production — but a key tenant of Lean is continuous improvement. Continually optimizing a process as it is developed (and long before it gets to a GMP production environment) equates to future proofing. It is much simpler to improve upon a process as it is developed and before it is validated for commercial production.
Additional Lean concepts:
- Reduced setup times: process liquids and buffers can be sourced externally and arrive already prepared, reducing downtime for production equipment.
- Standard work & operator training: first and foremost, this is a means of avoiding unnecessary production delays from engineers or operators, while empowering them to speak up if an issue arises. Standardizing wherever possible makes that training simpler, as well as simplifying purchasing and inventory (and subsequently shortening lead times).
- Reduced batch sizes: one‑piece flow in Lean translates to continuous pharmaceutical manufacturing. It enables better quality control, reduced footprint, and more uptime.
5. Maximize use of your pilot plants
This is the first place where engineering, clinical, commercial, regulatory, manufacturing, and process requirements are all explored together. Effectively locating bottlenecks and troubleshooting production issues at a small scale is key to ensuring that they do not pop up again at larger scales.
In addition to establishing production parameters, pilot plants (GMP or not) are the place to make sure that there are no capacity issues, that data and knowledge transfers are smooth, and that the equipment itself will scale without requiring new process parameters to be established. Focusing on the first scale‑up, from 10 L to 100 L, may be even more important than the scale‑up from 100 L to 10,000 L: that first scale‑up is when equipment types need to move from lab‑scale to production‑scale.
6. Opt for single-use equipment whenever possible
Another advantage of single‑use is that the facilities take less than a quarter of the time to build, because they are much less customized (see #7). Single-use facilities can generally be built in 12 – 18 months, compared to the 5 – 6 years it takes to build a large‑scale facility with the traditional reusable equipment. Although for large batch sizes, it often still makes sense to use stainless steel. But accurate forecasting of production demands will show that, particularly for biologics manufacturing, single‑use equipment often comes out ahead.
7. Standardize (preferably on single-use equipment)
It’s difficult to propose standardization in environments full of highly customized equipment. However, using standard equipment gives operators a common interface across skids, which then speeds up processing and reduces the possibility for human error. Servicing groups need to deal with fewer vendors; purchasing and inventory are pleased with the simplicity and shorter lead times; and IT loves that there are fewer security risks due to fewer data platforms in play, and that data integrity is greatly increased through less reformatting and transferring across platforms.
Choosing to standardize with single‑use equipment is especially beneficial. Single‑use has fewer materials variations, therefore requiring fewer FDA validations. It is also more flexible and can be used across a wider range of scales, making planning and purchasing easier in‑house and for your suppliers. Finally, it requires less training, because the same equipment can be used in more cases.
Together, this shows that standardization on single‑use equipment is particularly powerful — and explains the recent increase in single‑use prefabs.
8. Remember how different biologics are from traditional small molecule APIs
In 2017, biologics made make up 27% of new drug approvals in the US, up from 10% in 2007 — and they are projected to increase to 50% of the value of the top 100 products on the market by 2022. This market is very different than for small molecule drugs: biologics are primarily used for targeted therapies, precision treatments, and orphan drugs. Because these markets are so much smaller than for, say, ibuprofen (or even a biologic flu vaccine), less scale‑up is actually required. The manufacturing strategy for biologics is therefore often completely different than the manufacturing strategy for drug products in two key areas.
First, smaller batch sizes are both feasible and necessary. Equipment that is too big for the batch sizes will result in huge material losses, and because of the increased cost of manufacturing biologics, these losses are extremely costly. Using appropriately‑sized equipment for the smaller batches prevents losses. This opens the door to using primarily single‑use equipment, which is cheaper and more flexible than stainless steel alternatives.
Second, there needs to be more flexibility in manufacturing capabilities. It is likely that the equipment will need to be switched between various biologics, rather than being custom designed for a single process. The scalability of single‑use equipment provides another advantage here, if it later turns out that more of the product is necessary than originally forecast. As such, the same equipment could realistically be used for both early‑stage clinical trials and commercial production runs. This further reduces costs by eliminating facility and/or technical transfers, and the associated downtime and re‑validation.
9. De-risk your technology transfers
10. Integrate and automate early
If your pieces of equipment don’t communicate with one another, then operators need to configure data, technicians need to work with vendors on maintenance, and IT needs to work on basic integration functionalities. This scenario creates long changeover times while the data is dealt with and poses a serious risk to your data — which could close the door to regulatory approvals.
A 2019 survey reported that half of industrial companies had a data breach in the past year. Even something seemingly trivial can compromise data — a common example is an employee leaving a facility with a USB in their pocket.
Data breaches can be prevented by integrating equipment on a common network protocol and automating data collection. For instance, implementing an automatic batch historian reduces the risk of error significantly compared to manual data collection, while providing easy access to historic data for regulatory reviews. In combination with analytics software, it also becomes a powerful quality management tool.
11. Increase familiarity with the regulatory landscape
Not everybody in the organization needs to be an expert in validating processes with the FDA. However, everyone should be aware that if you need to change a piece of equipment, then you’ll need revalidation. This issue often arises when a piece of equipment is unable to scale with the process, necessitating replacement by a different piece that can handle larger production volumes.
If the engineers within an organization are all familiar with the regulatory framework and understand the time, cost, and work involved in validation, they can design systems with equipment specifically chosen for scalability and avoid unnecessary revalidation down the line.
12. Scale down effectively for efficient troubleshooting
Scaling down is just as important as scaling up, as it ensures you will be able to troubleshoot issues that inevitably arise throughout your process development — and troubleshooting in a small‑scale system that does not adequately replicate the mass transfer limits of the large system will not be particularly valuable. A scaled down system needs to replicate the oxygen transfer, agitation and aeration, power density, flows, shear rates, etc. of the larger system in order to be a useful tool.
13. Take advantage of operating in non-GMP environments when you can
Some pilot plants are validated GMP environments, others are not. When you are working in a non‑GMP pilot plant, it is much cheaper and easier to plan for and de‑risk your pharma scale‑up. So scale as far as possible in this environment, while keeping in mind that your end‑goal is GMP production.